What is "Pelvic Rehabilitation" and is it different from Pelvic Floor Physical Therapy?
May 21, 2022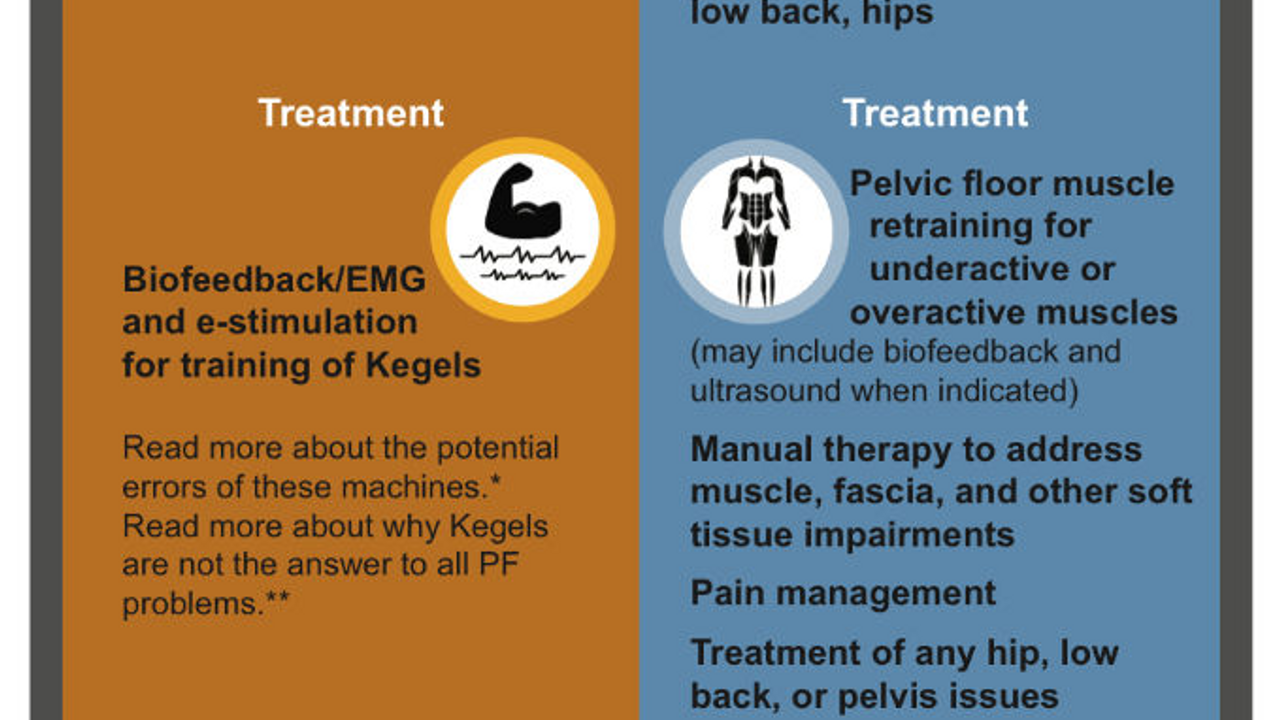
Author: Dr. Blair Green PT, DPT, OCS, PHC
I went to the gynecologist for my annual exam and I noticed that the practice was offering a new service – pelvic floor rehabilitation. I asked what it was and found out that the doctors had hired a company to provide their patients with a program to retrain the pelvic floor muscles, to help them with things such as prolapse, incontinence and pelvic pain. “Oh cool,” I thought. “I wonder which physical therapist is working here?” After asking, and checking the practice website, I found out that in fact the provider was not a physical therapist, but rather a nurse, who has been trained in EMG biofeedback and electrical stimulation. The advertised “pelvic floor rehabilitation” was no more than someone hooking patients up to a machine to help them learn how to contract their pelvic floor muscles better.
Many providers, and patients, associate pelvic floor dysfunction with weak muscles. In other words, if you leak – do Kegels; if you have prolapse, do Kegels; if you have pelvic pain, do Kegels. The biggest issue is that this “one size fits all” approach does not live up to its name. Sometimes, treating pelvic floor dysfunction may be simple and may only involve learning how to contract and relax muscles. Other times it may be complicated and require more assessment, examination and intervention strategies.
Historically, EMG biofeedback is widely utilized as an intervention for pelvic floor dysfunction. To read more about this tool, click here. Amy Stein, PT, who is the current president of the International Pelvic Pain Society, comments on the history of EMG biofeedback and its role in pelvic floor retraining (1). She describes the phenomenon of the “short or overactive pelvic floor” and how using only EMG biofeedback is not the current best practice to manage pelvic pain. Despite its use historically, our knowledge and skills have evolved over the last 15-20 years. Physical Therapists now use multiple intervention strategies, including manual stretching, soft tissue mobilization, relaxation strategies and muscle retraining.
Prendergast (2) discusses the role of physical therapy in the management of vulvodynia, a common pelvic pain syndrome. She emphasizes the assessment of skin, muscle, connective tissue, and other structures to determine the best course of care. She goes on to state that patients may present with similar symptoms but require very different treatment strategies. Again, this reinforces the emphasis on individualized care and the need for multiple choices of interventions.
This is not to say that EMG Biofeedback is a poor choice of intervention for underactive pelvic floor muscles. In fact, the literature does support pelvic floor muscle retraining to improve symptoms of stress urinary incontinence (3). It is simply to say this may not be the best choice. In other words, imagine you have a cut and are bleeding, a Band Aid will stop the bleeding, but a better option would be to clean the cut, use an antibacterial cream and cover it with a bandage.
I am grateful that my gynecologist and others are offering this service to patients. There was a time that they were not aware of pelvic floor physical therapy. This is step in the right direction. However, it is important that patients, as consumers of health care, have as much information available to them and can make the choice between good, better and best.
References:
- Stein A, Sauder S. On the backs of giants: the evolution of biofeedback in the treatment of vulvodynia. J Sex Med. 2017;14:1-2.
- Prendergast S. Pelvic floor physical therapy for vulvodynia. Obstet Gynecol Clin N Am. 2017;44:509-522.
- Hay-Smith EJC, Herderschee R, Dumoulin C, Herbison GP. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women (Review). The Cochrane Collaboration. 2011;12.
#pelvichealth #physicaltherapy #pelvicfloor #pelvicrehabilitation #womenshealth


